By Teresa Burns Murphy
On a sleepless Sunday night in late September 2021, I experienced pops of bone pain, teeth-chattering chills, and chest-constricting lung spasms. A little over a month earlier, I had been hospitalized for pneumonia. Fearing a return case, I phoned my primary care physician’s practice early the next morning. By ten o’clock, I was sitting in an exam room explaining my symptoms to the doctor.
“Any fever?” she asked.
“Low-grade,” I said.
“Headache?”
“Yes.”
“Shortness of breath?”
I could see where she was going with this line of questioning.
“You don’t think I could have COVID, do you?”
“I don’t think so, but we’re going to do a couple of tests and see,” she replied.
In short order, a nurse bustled in and swabbed each nostril twice—once for the rapid test and once for the two-day test. After that, I was dispatched to the lab for bloodwork and sent home to await the results.
Over the past ten years, I have spent a lot of time waiting for test results. On multiple occasions, I have been told that “suspicious masses” on my mammograms suggested that I might have breast cancer. Though I worried obsessively while waiting for the results of each biopsy, I didn’t cry. Luckily, those “suspicious masses” were not invasive breast cancer. When a “lesion” appeared on a brain MRI, I was told it might not be malignant, which meant there was a possibility that it could be malignant. I doomscrolled “brain cancer,” but I never once allowed myself to cry. Fortunately, the “lesion” turned out to be an “inflammatory process.” I didn’t even cry when I was told that test results confirmed that I had a chronic form of leukemia. Having leukemia has rendered me immunocompromised and is the reason I have received so many diagnostic tests over the years. Not only am I susceptible to infection, I am also at higher-than-average risk for every other form of cancer.
In the past, I have had to wait days, sometimes weeks, for various test results. This time, I didn’t have to wait long at all. I had been home for only a few minutes when the phone rang.
Apprehension seeping through her voice, the doctor said, “You tested positive for COVID.”
Because I am immunocompromised, my doctor prescribed REGEN-COV, an investigational treatment for mild to moderate symptoms of COVID-19 in patients who are at elevated risk for serious disease. The medication, a combination of two monoclonal antibodies (casirivimab and imdevimab) that block the virus from entering the body’s cells, is typically delivered as a single intravenous infusion. In order to be effective, REGEN-COV must be given within ten days of experiencing COVID-19 symptoms. I was told to get the infusion ASAP. As I listened to the doctor’s instructions for making the appointment to receive REGEN-COV, my mind whirred with worry and anger. How long had I had COVID-19? How and where did I get it? I had received the first two Pfizer jabs in mid-March and early April and had recently received a booster. I lived in an area with a high vaccination/low infection rate. And, I had severely limited my contact with other people.
Appointment to receive the infusion made for the next morning at seven thirty and isolated in an upstairs room, I went over all the places I had been (never without a mask) in the past two weeks. I had been to my daughter’s play—but that was outside and she had arranged for my husband and me to sit far away from the crowd. I had been to a garden center. That, too, was outside and I had dutifully worn my mask and kept my distance from other people. And, I had been in a doctor’s office where I, along with everyone else, wore a mask. That was it. My daughter and husband both tested negative, so I had to have gotten COVID-19 from someone (who was more than likely unvaccinated) in one of those three places.
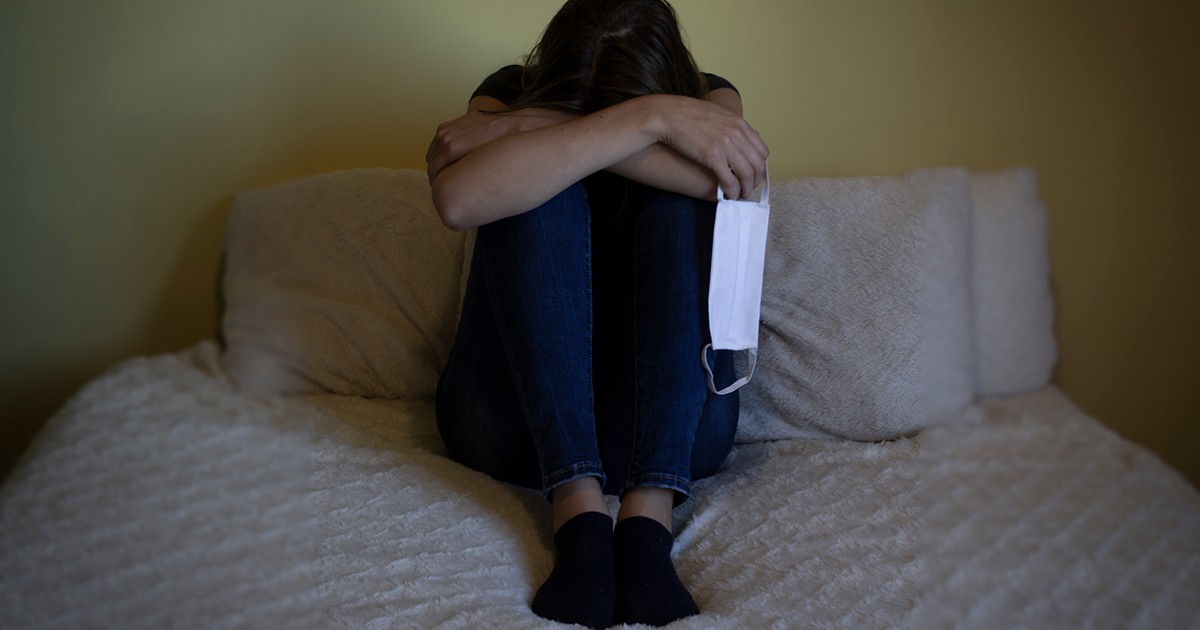
Thinking of how careful my family and I had been since the pandemic’s outset, I began to cry. As I accepted the reality that I had a breakthrough case of COVID-19, I wasn’t sure the tears, once they began to flow, were ever going to stop.